|
|
| ¡¡ |
|
Hyaluronic
Acid Knowledge |
|
|
Hyaluronic acid summary |
|
Hyaluro-nan's Biological
synthesis |
|
Cell receptors for hyaluronan |
|
Role of hyaluronan(hyaluronic acid) in cancer metastasis |
|
The Medical
applications of hyaluronic acid |
|
What are the differences
between glycolic acid, salicyclic acid, and hyaluronic
acid? What is the benefit of each type for skin? |
|
¡¡ |
|
¡¡ |
|
What are the differences
between glycolic acid, salicyclic acid, and hyaluronic
acid? What is the benefit of each type for skin? |
Glycolic Acid is the most active and beneficial of the
Alpha-Hydroxy-Acids in skin care and is made from
sugar canes. It is the only AH-A which is able to
penetrate through the cell walls by virtue of its small
molecular size. Once inside the cell, it will trigger
new formation of collagen and turn on the synthesis of
dermal glycosaminoglycans to plump up the cell and the
ground substances in the skin to reduce wrinkles on the
skins surface. Glycolic Acid also affects the newly
forming keratin cells at the bottom of the stratum
corneum causing the bulk of the stratum corneum to lift
off and separate from the underlying skin. This gives
the skin a much smoother look and feel.
Salicylic acid is a mild acid that works as a
keratolytic agent � it encourages the sloughing of dead
skin cells. It�s a safe, effective treatment for mild
acne, oily skin, textural changes and post-inflammatory
hyperpigmentation in patients of most skin types. Mild
acid solutions, such as salicylic acid and glycolic
acid, encourage the peeling of the top layer of skin and
the opening of plugged follicles, which helps
reestablish the normal skin-cell replacement cycle. For
milder acne, salicylic acid helps unclog pores to
resolve and prevent lesions. It does not have any effect
on the production of sebum or the presence of P. acnes
bacteria. Like many other topical acne treatments,
salicylic acid must be used continuously, even after
acne lesions have healed. Its effects stop when you stop
using it, so your skin will return to its uneven
shedding; pores become clogged, and acne returns.
Hyaluronic acid£¨Sodium
Hyaluronate for injection grade£© is a component
of connective tissue whose function is to cushion and
lubricate. Hyaluro-nan occurs throughout the body in
abundant amounts in many of the places people with
hereditary connective tissue disorders have problems
such as joints, heart valves and eyes. Hyaluronic acid
abnormalities are a common thread in connective tissue
disorders. Interestingly, they are also common
biochemical anomalies in most of the individual features
of connective tissue disorders such as mitral valve
prolapse, TMJ, osteoarthritis, and keratoconus.
Hyaluronic acid, or commercial preparations containing
hyaluronic acid, are in use or being studied to be used,
to prevent, treat or aid in the surgical repair for many
the types of problems people with connective tissue
disorders tend to have such as scar prevention, wrinkled
skin, cartilage damage and wound healing. |
|
Article Source: |
|
http://www.answerbag.com/q_view/4204 |
|
Back To Top |
|
¡¡ |
|
Hyaluronan's Biological
synthesis |
Hyaluronan £¨Sodium Hyaluronate for injection grade£©is synthesized by a class of integral membrane
proteins called hyaluronan synthases, of which
vertebrates have three types: H-AS1, H-AS2, and H-AS3.
These enzymes lengthen hyaluro-nan by repeatedly adding
glucuronic acid and N-acetylglucosamine to the nascent
polysaccharide as it is extruded via ABC-transporter
through the cell membrane into the extracellular space.
Hyaluro-nan synthesis (H-AS) has been shown to be
inhibited by 4-Methylumbelliferone (hymecromone,
heparvit), a 7-Hydroxy-4-methylcoumarin derivative.This
selective inhibition (without inhibiting other
Glycosaminoglycans) may prove useful in preventing
metastasis of malignant tumor cells. |
|
Article Source: |
|
http://en.wikipedia.org/wiki/Hyaluronan |
|
Back To Top |
|
¡¡ |
|
Cell receptors for hyaluronan |
So far, cell receptors that have been identified for HA
fall into three main groups: CD44, RH-AMM (Receptor for
Sodium Hyaluronate for
injection grade-Mediated Motility) and ICAM-1 (Intracellular adhesion
molecule-1). CD44 and ICAM-1 were already known as cell
adhesion molecules with other recognized ligands before
their H-A binding was discovered.
CD44 is widely distributed throughout the body, and the
formal demonstration of H-A-CD44 binding was proposed by Aruffo et al.in 1990. To date, it is recognized as the
main cell surface receptor for HA. CD44 mediates cell
interaction with H-A and the binging of the two functions
as an important part in various physiologic events,such
as cell aggregation, migration, proliferation and
activation; cell-cell and cell-substrate adhesion;
endocytosis of H-A, which leads to HA catabolism in
macrophages; and assembly of petircellular matrices from
HA and proteoglycan. Two significant roles of CD44 in
skin were proposed by Kaya et al.The first one is
regulation of keratinocyte proliferation in response to
extracellular stimuli, and the second one is the
maintenance of local Sodium
Hyaluronate for injection grade homeostasis.
ICAM-1 is known mainly as a metabolic cell surface
receptor for HA, and this protein may be responsible
mainly for the clearance of HA from lymph and blood
plasma, which accounts for perhaps most of its
whole-body turnover Ligand binding of this receptor,
thus, triggers a highly co-ordinated cascade of events
that includes the formation of an endocytotic vesicle,
its fusion with primary lysosomes, enzymatic digestion
to monosccharides, active transmembrane transport of
these sugars to cell sap, phosphorylation of GlcNAc and
enzymatic deacetylation. Like its name, ICAM-1 may also
serve as a cell adhesion molecule and the binding of HA
to ICAM-1 may contribute to the control of
ICAM-1-mediated inflammatory activation. |
|
Article Source: |
|
http://en.wikipedia.org/wiki/Hyaluronan |
|
Back To Top |
|
¡¡ |
|
Role of hyaluronan(hyaluronic
acid) in cancer metastasis |
As shown in Figure 1, the various types of molecules that
interact with hyaluro-nan can contribute to many of the
stages of cancer metastasis.
Hyaluro-nan synthases play roles in all of the
stages of cancer metastasis. By producing anti-adhesive
H-A(Sodium Hyaluronate for
injection grade), H-AS can allow tumor cells to release from the
primary tumor mass and if H-A associates with receptors
such as CD44, the activation of Rho GTPases can promote
epithelial-mesenchymal transition (EMT) of the cancer
cells. During the processes of intravasation or
extravasation, the interaction of H-AS produced H-A with
receptors such as CD44 or RH-AMM promote the cell changes
that allow for the cancer cells to infiltrate the
vascular or lymphatic systems. While traveling in these
systems, H-A produced by H-AS protects the cancer cell
from physical damage. Finally, in the formation of a metastatic lesion, H-AS produces HA(Sodium
Hyaluronate for injection grade) to allow the cancer
cell to interact with native cells at the secondary site
and to produce a tumor for itself.
Hyaluronidases (H-Aase or HYAL) also play many roles in
cancer metastasis. By helping to degrade the ECM
surrounding the tumor, hyaluronidases help the cancer
cell escape from the primary tumor mass and play a major
role in intravasation by allowing degradation of the
basement membrane of the lymph or blood vessel.
Hyaluronidases again play these roles in establishment
of a metastatic lesion by helping with extravasation and
clearing the ECM of the secondary site. Finally,
hyaluronidases play a key role in the process of
angiogenesis. H-A fragments promote angiogenesis and hyaluronidases produce these fragments.Interestingly,
hypoxia also increases production of H-A£¨Sodium
Hyaluronate for injection grade£© and activity of hyaluronidases.
The hyaluro-nan receptors, CD44 and RH-AMM, are most
thoroughly studied in terms of their roles in cancer
metastasis. Increased clinical CD44 expression has been
positively correlated to metastasis in a number of tumor
types. In terms of mechanics, CD44 affects adhesion of
cancer cells to each other and to endothelial cells,
rearranges the cytoskeleton through the Rho GTPases, and
increases the activity of ECM degrading enzymes.
Increased RH-AMM expression has also been clinically
correlated with cancer metastasis. In terms of
mechanics, RH-AMM promotes cancer cell motility through a
number of pathways including focal adhesion kinase (FAK),
Map Kinase (MAPK), pp60 (c-src), and the downstream
targets of Rho Kinase (ROK).RH-AMM can also cooperate
with CD44 to promote angiogenesis toward the metastatic
lesion. |
|
Article Source: |
|
http://en.wikipedia.org/wiki/Hyaluronan |
|
Back To Top |
|
¡¡ |
|
The Medical applications of hyaluronic
acid |
Hyaluro-nan£¨Sodium Hyaluronate
for injection grade£© is found in many tissues of the body, such as
skin, cartilage, and the vitreous humour. Therefore, it
is well suited to biomedical applications targeting
these tissues. The first hyaluro-nan biomedical product,
Healon, was developed in the 1970s and 1980s by
Pharmacia, and is approved for use in eye surgery (i.e.,
corneal transplantation, cataract surgery, glaucoma
surgery, and surgery to repair retinal detachment).
Other biomedical companies also produce brands of
hyaluronan(Sodium Hyaluronate for injection grade) for ophthalmic surgery.
In the late 1970s, intra-ocular lens implantation was
often followed by severe corneal edema, due to
endothelial cell damage during the surgery. It was
evident that a viscous, clear, physiologic lubricant to
prevent such scrapping of the endothelial cells was
needed.Endre Balazs patented a process for purifying
hyaluronic acid, a physiologic lubricant (which he
called Healon) from rooster combs in the early 1970s. At
first, Balazs saw Healon as a non inflammatory vitreous
substitute. Claus Dohlman had used Balazs¡¯ Healon in one
case in which the anterior chamber flattened after a
complicated corneal transplant. Although one might
imagine that the viscous hyaluronic acid would have
caused a rise in IOP, Dohlman reported no such rise in
his case. Since that time, Balazs had licensed the
synthesis process to Pharmacia, a Swedish drug company.
Although Pharmacia saw no market for a vitreous
substitute, when their scientists figured out a way to
increase the viscosity of hyaluronic acid£¨Sodium
Hyaluronate for injection grade£© , they felt it
might work as an injectable agent in the treatment of
both human and equine arthritis. The equine arthritis
market proved to be small and the treatment of human
osteoarthritis produced only marginal improvement and so
Pharmacia decided to abandon Healon. At this time, David
Miller realized that Healon was the lubricant needed by
the eye surgeon.
Balazs arranged to have Pharmacia send 20 sterile vials
to Dr. David Miller for rabbit experiments. By 1976,
Miller and colleagues published a study showing that
Healon worked well in protecting the rabbit corneal
endothelium during IOL implantation. With a new possible
use for Healon. Miller met with Pharmacia and performed
a lens extraction and IOL implantation using Healon in a
rabbit eye. The demonstration ignited an new enthusiasm
for eye surgery with Healon. A small human pilot study
at Boston¡¯s Beth Israel Hospital by Miller confirmed
Healon¡¯s beneficial effects.
In a large, well-controlled clinical trial, Dr. Robert
Stegmann, of Pretoria, South Africa was able to quantify
the advantages of Healon in IOL implantation by showing
significantly higher post operative corneal endothelial
counts in the Healon eyes as opposed to the controls.
The FDA quickly approved Healon as a surgical device in
1980 and Healon was successfully launched. By the year
2009, an estimated quarter of a billion patients had
benefited from the useful properties of Healon in eye
surgery.
In 1992, Miller and Stegmann received the Innovators
Award by the American Society of Cataract and Refractive
Surgery for developing the use of healon in repairing
injured eyes.
Hyaluro-nan is also used to treat osteoarthritis of the
knee. Such treatments, called viscosupplementation, are
administered as a course of injections (Sodium
Hyaluronate,Sodium Hyaluronate for injection grade) into the knee
joint and are believed to supplement the viscosity of
the joint fluid, thereby lubricating the joint,
cushioning the joint, and producing an analgesic effect.
It has also been suggested that hyaluro-nan has positive
biochemical effects on cartilage cells. However, some
placebo-controlled studies have cast doubt on the
efficacy of Hyaluronic Acid injections(Sodium Hyaluronate for injection grade), and hyaluro-nan is
recommended primarily as a last alternative to surgery.
Oral use of hyaluronan has been lately suggested,
although its effectiveness needs to be demonstrated. At
present, there are some preliminary clinical studies
that suggest that oral administration of Hyaluro-nan has
a positive effect on osteoarthritis, but it remains to
be seen if there is any real benefit to the treatment.
Dry, scaly skin (xerosis) such as that caused by atopic
dermatitis (eczema) may be treated with a prescription
skin lotion containing sodium hyaluronate as its active
ingredient.
Due to its high biocompatibility and its common presence
in the extracellular matrix of tissues, hyaluronan is
gaining popularity as a biomaterial scaffold in tissue
engineering research.In particular, a number of research
groups have found that hyaluro-nan's properties for
tissue engineering and Regenerative medicine are
significantly improved with crosslinking, producing a
hydrogel. This added feature allows a researcher to form
a desired shape as well as to deliver therapeutic
molecules into a host. Hyaluro-nan can be crosslinked by
attaching thiols (trade names: Extracel, HyStem),
methacrylates,and tyramines (trade name: Corgel).
Hyaluro-nan can also be crosslinked directly with
formaldehyde (trade name: Hylan-A) or with divinyl
sulfone (trade name: Hylan-B).
In some cancers, hyaluro-nan levels correlate well with
malignancy and poor prognosis. Hyaluro-nan is, thus,
often used as a tumor marker for prostate and breast
cancer. It may also be used to monitor the progression
of the disease.
Hyaluronan (Sodium Hyaluronate for injection
grade) may also be used postoperatively to induce
tissue healing, notably after cataract surgery. Current
models of wound healing propose that larger polymers of hyaluronic acid appear in the early stages of healing to
physically make room for white blood cells, which
mediate the immune response.
Hyaluro-nan has also been used in the synthesis of
biological scaffolds for wound-healing applications.
These scaffolds typically have proteins such as
fibronectin attached to the hyaluronan to facilitate
cell migration into the wound. This is particularly
important for individuals with diabetes suffering from
chronic wounds.
In 2007, the EMA extended its approval of Hylan GF-20 as
a treatment for ankle and shoulder osteoarthritis pain.
Hyaluro-nan is also used in anti-adhesive products such
as Hyalobarrier, widely used in pelvic and abdominal
surgery to prevent post-operative adhesions. |
|
Article Source: |
|
http://en.wikipedia.org/wiki/Hyaluronan |
|
Back To Top |
|
¡¡ |
|
Hyaluronic acid summary |
Hyaluro-nan (HA,also called hyaluronic acid or hyaluronate) is
a glycosaminoglycan distributed widely throughout
connective, epithelial, and neural tissues. It is one of
the chief components of the extracellular matrix,
contributes significantly to cell proliferation and
migration, and may also be involved in the progression
of some malignant tumors. The average 70-kg man has
roughly 15 grams of hyaluro-nan in his body, one-third of
which is turned over (degraded and synthesised) every
day. Hyaluro-nan is a common ingredient in skin care
product, and the branded version Restylane is used as
injections (Sodium Hyaluronate,Sodium Hyaluronate for injection grade) to temporarily smooth wrinkles by adding
volume under the skin or the brand Macrolane to increase
breast size by adding volume using a natural tissue
chemical.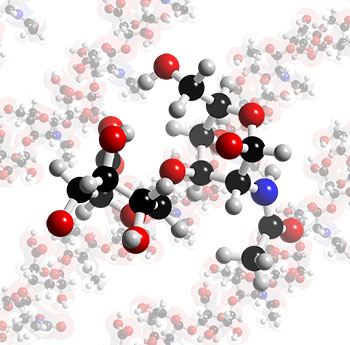
Hyaluro-nan is a polymer of disaccharides, themselves
composed of D-glucuronic acid and D-N-acetylglucosamine,
linked together via alternating ¦Â-1,4 and ¦Â-1,3
glycosidic bonds. Hyaluro-nan can be 25,000 disaccharide
repeats in length. Hyaluro-nan is an important component
of articular cartilage, where it is present as a coat
around each cell (chondrocyte). When aggrecan monomers
bind to hyaluro-nan in the presence of link protein,
large highly negatively-charged aggregates form. These
aggregates imbibe water and are responsible for the
resilience of cartilage (its resistance to compression).
Hyaluro-nan is also a major component of skin, where it
is involved in tissue repair. When skin is excessively
exposed to UVB rays, it becomes inflamed (sunburn) and
the cells in the dermis stop producing as much
hyaluro-nan, and increase the rate of its degradation.
Hyaluro-nan degradation products also accumulate in the
skin after UV exposure. Hyaluro-nan also contributes to
tissue hydrodynamics, movement and proliferation of
cells, and participates in a number of cell surface
receptor interactions.
Hyaluro-nan is naturally found in many tissues of the
body, such as skin, cartilage, and the vitreous humor.
It is therefore well suited to biomedical applications
targeting these tissues. The first hyaluro-nan biomedical
product, Healon, was developed in the 1970s and 1980s by
Pharmacia, and is approved for use in eye surgery. In
2003 the FDA approved hyaluro-nan injections (Sodium Hyaluronate,Sodium Hyaluronate for injection grade) for filling
soft tissue defects such as facial wrinkles. Restylane
is a common trade name for the product, injections of
Restylane temporarily smooth wrinkles by adding volume
under the skin, with effects typically lasting for six
months, it is also used to give volume to lips. More
recently, Macrolane, another trade name has been used as
a non-surgical body shaping treatment that can naturally
regenerate body contours. This can be used for large
volume restoration and shaping of body surfaces, for
example, calves and buttocks. Macrolane can also even
out discrepancies in the skin surface, for example those
caused by liposuction. In 2008, Macrolane has started to
be used for breast shaping, and is aimed to be used for
women whom have asymmetry, loss of volume as a result of
breast feeding or weight loss, or under-developed
breasts. Marketing suggests it is suitable for women to
increase by a cup size without the need for surgery. Of
course, the body naturally processes hyaluronan£¨Sodium Hyaluronate for injection grade£©, so
shaping only last for 12-18 months and top-ups would be
required to retain shape or smooth skin. |
|
Article Source: |
|
http://www.3dchem.com/molecules.asp?ID=425 |
|
Back To Top |
|
¡¡ |
¡¡ |
| ¡¡ |
|